Can COVID-19 cause a stroke?
At first, Pam Hutton thought her case of COVID-19 would be no big deal.
“I just thought I had allergies, honestly,” the 44-year-old Canton woman said.

Pam Hutton
She and her husband had tested positive for the illness caused by the novel coronavirus in April of 2020. After a few days of isolating at home and monitoring their symptoms, Pam decided to seek medical attention when her oxygen levels – measured by a pulse oximeter – began to drop.
She was admitted to the hospital in her hometown, and her symptoms became worse.
“I had shortness of breath, loss of smell, loss of taste, massive headaches – off the chart headaches. I’ve had headaches all my life, but I had never felt that kind of pain ever. It was so excruciating,” Pam said.
Within two days of arriving in the hospital, Pam had a stroke – a complication that a small percentage of people infected with COVID-19 experience.
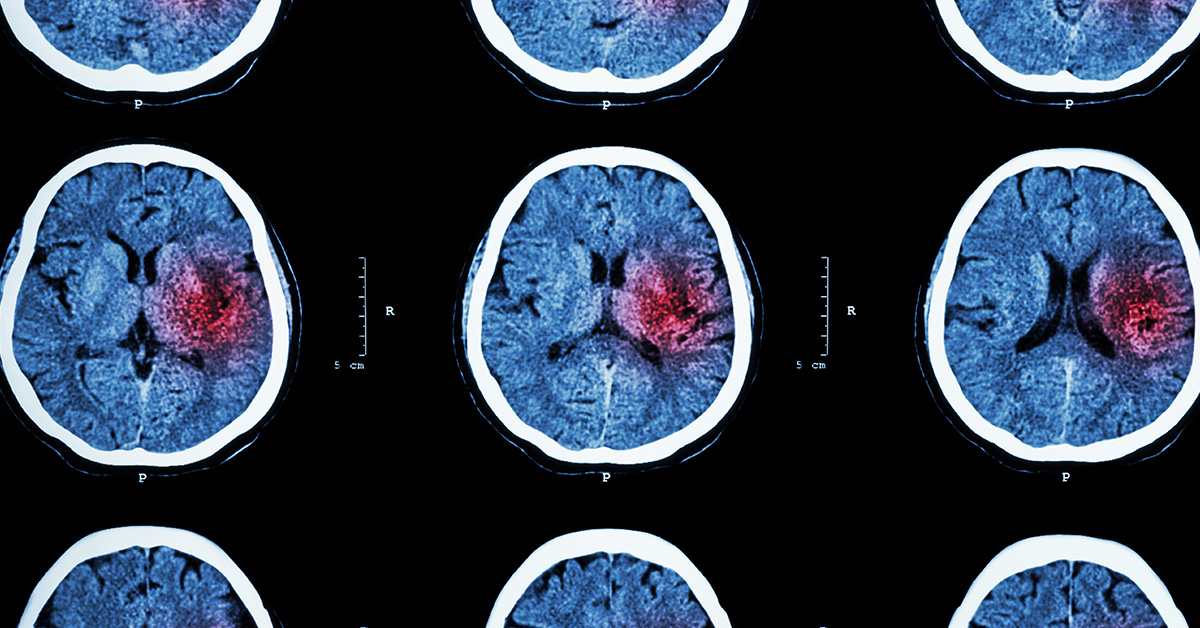
What causes a stroke?
Strokes happen when the brain’s blood supply is cut off, such as when a blood clot or blockage occurs (ischemic stroke) or an artery in the brain ruptures (hemorrhagic stroke). Ischemic strokes are much more common than hemorrhagic, and this is the type of stroke Pam experienced.
“There are three ways a blockage of an artery can occur. One is an injury to the artery itself, usually a trauma. The other way is an anatomical abnormality of those blood vessels, and sometimes we discover that after the fact,” said Deepak Nair, MD, an OSF HealthCare neurologist who specializes in stroke and critical care. Dr. Nair was one of several neurologists involved in Pam’s care at OSF HealthCare Saint Francis Medical Center in Peoria.
“The third is something in the blood that is increasing the risk of clotting, and that’s where COVID-19 comes in.”
The link between COVID-19 and stroke
Pam is just one of the handful of patients Dr. Nair has seen in several months who have had a stroke after a COVID-19 diagnosis. Most of them, he said, had an underlying risk factor that may have put them at increased risk of a stroke before their exposure to the novel coronavirus.
There is enough evidence that physicians and researchers suspect a connection between COVID-19 and stroke, though the relationship and risks are not yet clear.
“We do know that there are some specific mechanisms that COVID-19 is causing that increase the chances of stroke. But there are probably multiple factors at play, and many of those are not understood,” Dr. Nair said.
In Pam’s case, there appeared to be two factors at play: the formation of a large blood clot and the narrowing of one of her arteries.
The effects of COVID-19
A virus such as the one that causes COVID-19 can cause changes in the way our cells function. It also triggers our immune system’s response, which naturally produces chemicals in our bodies that cause more changes to how we normally function.

Pam Hutton and Family
These biological changes can increase the risk of forming a blood clot, increasing the risk of stroke.
It’s also plausible, Dr. Nair explained, that increased clotting in the blood could have been a complication of a medication used to treat COVID-19. This is not unique to COVID-19 and has been observed in other infections that can cause serious illness.
All of this has to be taken into context with a person’s health history and underlying conditions. One risk factor alone is usually not enough to cause a stroke.
“It’s very unusual for us to have a singular reason that somebody had a stroke. When we see patients of stroke, they already have accumulated multiple risk factors, and it’s challenging to say how much each one contributed,” Dr. Nair said.
While Pam’s age was not a major risk factor at just 44 years, and she was otherwise healthy, she was treated for a brain tumor.
Reducing risk
While it’s difficult to say exactly how an illness known for attacking the respiratory system led to Pam’s stroke, she and Dr. Nair agree that outcomes like hers are a good reason to try to prevent COVID-19 infections.
Dr. Nair stressed that anyone with risk factors for stroke – diabetes, a history of smoking, high blood pressure, or high cholesterol – would be smart to protect themselves from COVID-19 and complications from the disease.
While Pam has recovered from COVID-19, she still has some lingering effects of stroke – numbness and some difficulty finding the right word at times.
“I’m feeling OK. I’m doing things with my mind like puzzles, word searches, and doing everything I can on my end to get therapy,” she said.
And she’s taking the COVID-19 pandemic more seriously.
“I wanted to share my story for people who don’t think this is real, who think this can’t happen to a 44-year-old woman,” she said.
Though she knows it’s unlikely she could be infected again with COVID-19, she wears a mask whenever she leaves her home, even to visit family, and encourages others to do the same.