NeuroHealth Lab making strides
Our NeuroHealth Lab was one of seven OSF Innovation Labs launched in 2020 to focus on solving complex issues the Ministry faces. This builds on the work we have done over the last couple of years to find new ways to assess, identify and treat people with neurological disorders like ALS, dementia, Parkinson’s disease, Multiple Sclerosis and others.
Our goal is to ensure we can keep up with the demand for care as more people are diagnosed with neurological conditions in the future while the shortage of neurologists continues to grow.
Our work includes developing next-generation solutions to transform how neurological care is delivered and improve triage and access to care. Another part of our work is to build neuro exam trainers that give medical professionals in training the practice they need to detect neurological conditions. We are excited to report some of the advancements we have made over the last year.
Ongoing projects
Digitizing the neurological screening examination
As part of this project, we are building a platform that will use digitized neurological exam information and artificial intelligence technology to help clinicians detect and diagnose neurological conditions. It will also support triage and care for patients regardless of examination location.
In partnership with computer science engineers at the University of Illinois Urbana-Champaign, we’ve created a system that uses video to track and measure the movements of individuals undergoing neurologic assessments. This could help clinicians diagnose and care for people experiencing neurologic conditions by consistently identifying normal or abnormal movement.
Over the last year, we recorded four visualized neurologic exam findings on 21 healthy volunteers who produced both normal functions as well as different types of simulated impairments. Computer scientists on the team analyzed those recordings. They then wrote programs that use pose estimation to place skeletons on the people who were recorded to track their movements, identify features of what was seen, and measure the exam findings.
This gave us a proof of concept, which is an exciting first step. Most recently, our team received additional funding to start recording actual OSF patients, collect examples and test how this system will work. We hope to record at least 100 patients who have Parkinson’s, Multiple Sclerosis or other neurologic conditions that affect some portion of the neurologic exam that we can see. We then will develop a way to measure those findings and determine how to incorporate them more clinically.
Training devices
We know medical students and residents have a difficult time learning to examine patients for possible neurological conditions like ALS because they most likely won’t encounter many individuals with these illnesses as part of their training. As a result, new physicians and other clinicians don’t have the experience they need to determine when an individual might be displaying exam findings of abnormal neurologic function.
One of the ways we’re trying to improve ALS care is by earlier diagnosis. It typically takes 11 to 13 months from the onset of symptoms to when ALS is formally diagnosed. On average, patients will see three other clinicians before they get to the neurologist who diagnoses them.
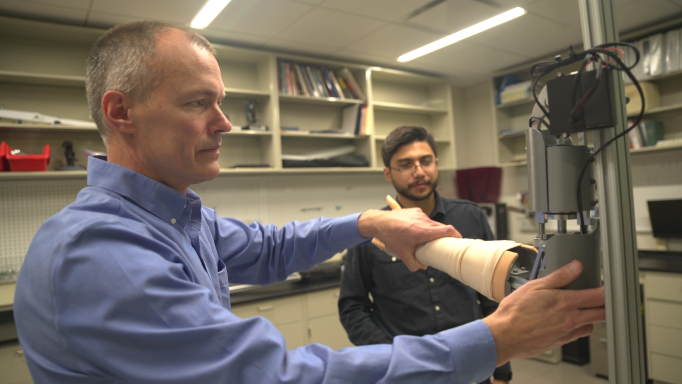
In collaboration with U of I engineers, we have developed a variety of robotic simulators designed to help health care providers-in-training learn to identify different abnormalities. These training devices will give clinician‐learners the opportunity to practice feeling and identifying abnormal muscle behaviors as often as they need to feel comfortable with the process.
So far, we’ve developed a hydraulic spasticity simulator that allows users to understand what this type of muscle tightness feels like and an electric motored rigidity simulator that imitates Parkinson’s muscle stiffness. We’re creating new arm and hand weakness simulators. And we’ve produced an ankle clonus task trainer that mimics a reflexive repetitive movement of the foot. Clonus can be seen with ALS and other conditions affecting the brain or spinal cord pathways for muscle movement.
The overall goal of creating these simulators is to standardize and provide more consistent learning experiences to medical trainees. We hope this translates to patients receiving better screening and detection of neurologic conditions causing spasticity, weakness or rigidity sooner, meaning faster diagnosis and starting of treatments.
Partner with us
We wouldn’t be as far as we are today without the help of the Jump Applied Research for Community Health through Engineering and Simulation (Jump ARCHES) endowment program and donors who continue to invest in our work.
If you are interested in learning more about the NeuroHealth Lab, participating in certain aspects of the journey or if you want to invest or partner, contact us today.